Deep brain stimulation can offer relief to people suffering from a variety of disorders.
It started with a slight tremor in one of Carol Javernick’s hands. Then there was pain in the leg on that same side. Any exercising soon left her out of energy. In time, she was unable to walk more than a few steps. Her descent into Parkinson’s disease was long and miserable.
Javernick, who lives in Westminster, Colo., eventually got relief with medicine. But it didn’t last long. And the drug caused other problems. Sometimes her leg would kick uncontrollably, ruining her newfound freedom. That’s when her doctor suggested she try something different. He wanted to place thin wires deep into her brain. These wires would carry battery-powered electrical signals. Called deep brain stimulation, this procedure has helped many patients with Parkinson’s disease return to more normal lives for years.
Javernick underwent a 10-hour surgery to implant the wire leads. After the doctors opened her skull, they woke her up. “My neurologist was there and would test me cell by cell with stimulation to see where to put the electrodes,” she recalls. Some spots caused her muscles to tighten up or her legs to kick. The doctors eventually found the best places for the leads. The medical team then ran the wires under Javernick’s skin. These were later attached to a battery pack implanted in her chest.
After two weeks of recovery, she spent long days in her doctor’s office. He connected the wires to a battery. Then he adjusted the electrical signals and ran some movement tests to see how well she did. The signals needed to be strong enough to stop the effects of Parkinson’s. But they could not be so strong that they caused other types of uncontrolled movement.
“When they turned [the battery] off and on it was a weird experience — almost like a jolt to my brain,” Javernick recalls. “Some settings would cause me to laugh and others made me tired.” Still others triggered those uncontrolled tremors. But the team finally found one that worked. Three years later, she is going strong. “I am not symptom-free,” she says. “But I am able to walk and participate in many activities that I was unable to do before.”
Deep brain stimulation turned Javernick’s life around. It’s begun doing the same for people with several other diseases and disorders, too. These include obsessive-compulsive disorder and depression. For many people, zapping the deep brain can restore a sense of normalcy.
Mixed signals
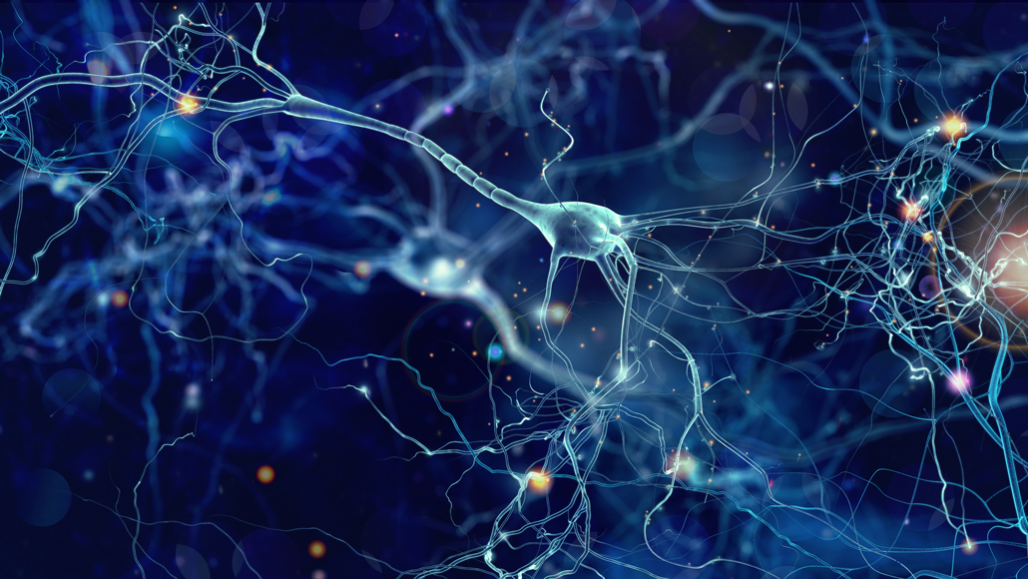
Parkinson’s disease is one of many diseases and disorders caused by signaling problems in the brain. The brain is made up of billions of neurons. These neural cells “talk” to each other by sending signals to neighboring cells. They do this by releasing chemicals called neurotransmitters. These chemical messengers travel across a gap between the cell that’s “talking” and the one that’s “listening.”
When the neurotransmitters attach to the outside of the listening cell, they trigger an electrical pulse in the second neuron. That signal zips along the length of the neuron. As it reaches the far end of the neuron, it causes the cell to release neurotransmitters to still other cells. This rapid-fire signaling is how our brains tell our muscles how to move — and how quickly. It’s also how our thoughts develop.
Many of those connections lead to still more electrical signals zipping through the brain. And those signals then release neurotransmitters to other neurons.
Some neurons, however, have the opposite effect. Instead of causing the next neuron to “fire,” an incoming neurotransmitter may prevent it from doing so. This is essential for keeping messages clear. When too many neurons fire at the same time, signals can get crossed. Problems can arise. Jittery movements, for example. Or obsessive thoughts. Even a deep sadness that never seems to go away.
In some people, deep brain stimulation can fix those mixed signals. Electrodes must be placed in very precise regions in the brain — even at specific cells. When a doctor turns on a battery-powered system, it begins releasing high-frequency electrical signals. These signals interfere with the electrical signals that are occurring naturally — but in error.
Surprisingly, scientists aren’t sure exactly how deep brain stimulation works. Some think it acts to inhibit, or prevent, some neurons’ firing. Others that it causes cells to fire. There’s some evidence it can do both. But Satomi Chiken and Atsushi Nambu think there might be another explanation. Chiken and Nambu work at the National Institute for Physiological Sciences in Okazaki, Japan. As neurophysiologists (Nur-oh-fiz-ee-OL-oh-gizts), they study how nerve cells work.
Deep brain stimulation may work by disrupting neural signals, their experiments suggest. When one cell sends signals to another cell over and over, the two cells create a strong link. After a while, it takes less of the chemical to make the second cell fire. One might think of them as becoming wired together.
That’s a problem if that new wiring is causing movement issues or obsessive thoughts. Chiken and Nambu think deep brain stimulation helps to disconnect cells that have become mistakenly wired.
The abnormal activity of cells is what causes symptoms, Nambu says. Disconnecting them “prevents the flows of such abnormal activity.”
Overcoming obsession
Deep brain stimulation has long been used for movement disorders. In the last 15 years, it also has become a way to treat certain mental-health problems. Among them: obsessive-compulsive disorder, or OCD.
Patients with OCD have unwanted thoughts or feelings much of the time. They might worry about germs or fear that they have left the oven on or some door unlocked. These thoughts or feelings become obsessive, meaning they take over their attention.
To deal with those feelings, people with OCD repeat the same action multiple times. They might wash their hands again and again, for example. Or check repeatedly that they turned the oven off. They can feel compelled — driven — to do these actions. For some people, those thoughts and actions become so all-consuming that they can’t leave the house or talk to people.
Most people with OCD are helped by medicines and behavioral therapy. But one in 10 of them won’t respond to such treatments. For them, deep brain stimulation may be an answer.
Just like Javernick’s experience, these patients undergo surgery to implant wire leads. The only difference is where in the brain those wires will go. Afterward, patients may spend weeks or months working with a neurologist to find the setting that reduces their symptoms without causing too many side effects.
Some people may get immediate relief, note Sanneke de Haan and Damiaan Denys. Both work in the Netherlands. De Haan is a psychiatric researcher at the University of Tilburg. Denys is a psychiatrist at the University of Amsterdam. The pair interviewed 18 adults who had deep brain stimulation to treat their OCD. The researchers wanted to learn what these people had experienced with the treatment.
The biggest change: less anxiety. Those obsessive, worrying thoughts lifted, sometimes just minutes after the electrodes were turned on. For most people, their thoughts didn’t go away completely. And not right away for anyone. But many said it felt as though a weight had been lifted. They no longer felt like they needed to obsess over things.
They also felt more cheerful, happy and optimistic. No longer weighed down by their constant worries, they felt able to let things go. They reported feeling more confident, stronger and assertive. This changed the way they interacted with other others — or interacted at all, in some cases. Many were able to do everyday tasks, such as grocery shopping. Until recently, that might have been impossible.
“Deep brain stimulation can cure the compulsive disorder in some patients,” Denys says. In one in five patients the symptoms almost completely disappear. Before treatment, he says, some patients might “clean their homes 12 to 16 hours a day in a compulsive manner.” After deep brain stimulation, that ritual might drop to only 15 minutes a day.
It’s not a perfect solution. Half of the patients had fewer symptoms. But usually the symptoms did not fully disappear; they only decreased by about half. Those that constantly cleaned before treatment, for instance, might spend only six to eight hours at it afterwards. Still, deep brain stimulation offered them some help, Denys says. “Although they are unable to take up normal life, the reduction in symptoms significantly improves their quality of life.”
Undoing depression
Deep brain stimulation also has begun to help some people with severe depression. More than just sadness, major depression is a serious disorder. People who suffer from it may feel hopeless. Some may lose interest in hobbies, their work or their friends and family. Many have trouble eating and sleeping. Some find it hard to think, speak or move. Although many people with depression can be helped by drugs, those medicines don’t work for everyone.
Helen Mayberg wanted to help those who didn’t respond to drugs. A neurologist, or brain specialist, Mayberg works at Emory University in Atlanta, Ga. She first used deep brain stimulation with six depressed patients in 2005. Five patients reported feeling somewhat better within a day or two. They slept better. They had more energy. They reported becoming more active and finding a renewed interest in many aspects of their life. Six months later, three of these four were no longer depressed. But one patient never felt better. Another improved for a while, then worsened.
Those early findings were promising. But a large follow-up study didn’t find that deep brain stimulation helped. “It felt like a disappointment,” says Patricio Riva Posse. He is a psychiatrist at Emory who works with Mayberg. It was frustrating, he says, because in smaller trials, “many patients and doctors had seen good results.”
Why deep brain stimulation helps some and not others is now under investigation. One possibility is that the wire leads were not in the right location for those who didn’t get better. Mayberg and Riva Posse have been trying to figure out how to put the leads in the spots that should offer the most help. Finding those spots is tricky, because they’re different in each patient.
In a 2013 study, the Emory team found one possible way to help. Patients who responded well to deep brain stimulation had their leads in specific bundles of neurons. These bundles, or tracts, connect specific parts of the brain. Last year, the team tested this idea in 11 patients. Before surgery, their brains were scanned using magnetic resonance imaging, or MRI. This gave the researchers a high-resolution image of all areas of each person’s brain. They then used special software that located those tracts in each scan. Afterward, they targeted a small, 3-millimeter spot within that tract as the best site for the wire leads.
During surgery, they placed four leads in the target site on each side of the brain. During the operation, they also tested the locations and how well they worked. “Patients were awake during the operation,” Riva Posse explains. “The doctors turned on the stimulation in the operating room.” As they tested each lead, the patients reported how they felt. Some felt “lighter” or “warmer.” That appeared to signal their depression was lifting.
After the patients had recovered from surgery, the team once more scanned each person’s brain. This time, they used a special type of X-ray called a CT scan. This gave them a precise image of where each lead was located. They then matched up the MRI scan and the CT scan. They looked for the single lead on each side of the brain that matched the positive response in the operating room. That was the lead they turned on. The team then followed the patients for more than a year.
Nine patients improved, and for six of them, their depression disappeared. Some responded quickly. Others took more than a year to really feel good again.
And while deep brain stimulation played an important role, it was not the only thing that helped many patients. During weekly meetings with a psychologist, each patient was taught how to recognize negative thoughts. They also learned how to look at those thoughts critically. And how to overcome them. This whole process is known as cognitive behavioral therapy, or CBT.
It was an essential part of their recovery, Riva Posse says. “These patients have been ill for a very long time.” They have unhealthy habits that can delay their recovery, he says. The patients had all tried CBT before. But when practiced together with deep brain stimulation, it seemed to help more. “They are able to engage better in the therapy,” Riva Posse says. And that made it easier for them to undo the bad habits they had built up over years of depression.
Deep brain stimulation is invasive, Riva Posse notes. Most patients respond to less invasive treatments, such as talk therapy and medication. But not all. For these others, deep brain stimulation may at last bring recovery, he says. “We are grateful to have been able to treat patients that had been ill for many years.”
That said, deep brain stimulation may not be a long-term solution for everyone. “Deep brain stimulation is not a cure,” Javernick says of her Parkinson’s disease. Eventually, the electrodes will be unable to stop her tremors. And the therapy is new for many other disorders. Researchers don’t yet know how long the effects of that brain stimulation will last. But for now, it seems to be a promising possibility for people with several seemingly untreatable brain disorders.











![Hotstar Premium Cookies 2019 [*100% Working & Daily Updated*] Hotstar Premium Cookies 2019 [*100% Working & Daily Updated*]](https://tahav.com/wp-content/uploads/2019/11/Hotstar-Premium-Cookies-Free-100x70.jpg)



