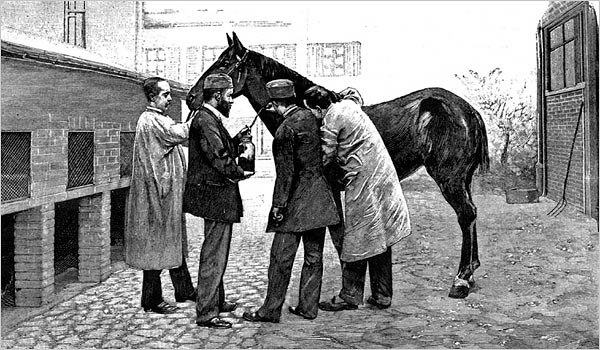
If you ever get diphtheria, a respiratory disease caused by a toxin-producing bacterium, your best hope of surviving is based on a treatment developed in the 19th century that relies on horses to produce an antitoxin. Back then, it was a breakthrough so profound that it won the discoverer, German physiologist Emil von Behring, the first ever Nobel Prize in Physiology or Medicine. But today, the method—which harvests antibody-rich serum after injecting the diphtheria toxin into horses—is widely seen as antiquated, and some find it cruel, given how the animals used are sometimes treated. (The toxin itself does not seem to seriously harm the horses.)
Now, a group of scientists funded by an animal welfare consortium has used lab-grown cells to make human antibodies that they say could finally replace the ones produced in horse serum. Several of the new antibodies combined protected guinea pigs from the effects of the diphtheria toxin injected into the skin; the scientists hope trials in humans will be next.
“This is a great piece of work that responds to the international need for a replacement” for horse serum, says Mark Klempner, who works at MassBiologics, a nonprofit group at the University of Massachusetts Medical School that is also developing a horse-free way to make diphtheria antitoxin.
The toxin produced by the bacterium that causes diphtheria, Cornybacterium diphteriae, kills cells and leads to the build up of dead tissue in the respiratory tract that forms a dense, gray layer. The “strangling angel,” as it was called in the 19th century, once killed hundreds of thousands of children worldwide each year. Routine childhood immunizations with an inactivated form of the toxin reduced the number of cases to several thousand annually—mostly in children who missed their vaccinations. Antiserum, the toxin-thwarting serum purified from horse blood, is still the standard treatment, in addition to antibiotics.
There are hardly any producers of antiserum left, however. Even when it’s available, batches can vary from horse to horse. And People for the Ethical Treatment of Animals (PETA) and other organizations have criticized what they say is inhumane treatment of horses at the producing facilities. Another downside: In up to 5% of cases, the patient’s immune system reacts against the horse antibodies, a life-threatening side effect called “serum sickness.”
For all of those reasons, the PETA International Science Consortium, created by various national PETA bodies, offered funding for alternatives, And in 2016, Michael Hust of the Technical University of Braunschweig used some of that funding to set out to produce human antibodies against the diphtheria toxin using an increasingly popular lab technique called “phage display.” The team immunized three people against diphtheria using the standard vaccine and 1 week later collected blood to isolate the immune cells that make antibodies that target the toxin. Isolating the antibodymaking genes from these select cells, they transferred them to phages—bacteria that infect viruses—to build up a library of millions of the phages in which each phage presents a different antibody on its surface. They then picked the phages whose antibodies bound most tightly to the diphtheria toxin and tested those antibodies’ activity against the toxin in cell culture and guinea pigs. (The guinea pig work was not funded by the PETA International Science Consortium.)
Even the best antibody alone did not protect the animals from the effects of diphtheria toxin, but when researchers combined two or three of the antibodies, they did. “The antibodies described here are promising candidates” to replace horse antiserum, the scientists write in a paper published today in Scientific Reports.
The antibodies will have to be tested in humans, however, a procedure that will take years and cost millions of dollars. Given that diphtheria cases are rare, companies have shown minimal interest in the past. “The further development is a challenge,” Hust acknowledges. “This kind of therapeutic can only be developed with the support of philanthropic donors and different stakeholders.” But the PETA International Science Consortium has been in discussions with several Indian drug companies interested in carrying the project forward, says the consortium’s Jeffrey Brown, one of the paper’s authors. “The project partners are in discussions with global health authorities who may also be able to support further clinical development,” he wrote in an email.
Meanwhile, a single-antibody treatment developed through directly screening human antibodies by MassBiologics appears to be further ahead. It has just been tested in a phase I clinical trial, which typically establishes safety, not efficacy. Although the data from that trial aren’t published yet, Klempner says discussions are already ongoing with the U.S. Food and Drug Administration to replace an aging stockpile of diphtheria antiserum from horses kept at the U.S. Centers of Disease Control and Prevention. The stockpile is officially expired and doses are only offered as an experimental therapy.
MassBiologics’s antibody, called S315, has been tested in more stringent animal models than the German team used, Klempner says. And one advantage of having a single antibody is that it will be cheaper than a combination of two or three antibodies, he says, adding that it should also be comparable in cost or less expensive than the horse serum treatment.
Hust, meanwhile, has set his eyes on developing lab antibodies to replace another horse-produced remedy, again funded by consortium: The antivenom used to treat bites by black widow spiders. Although those bites are not usually life-threatening and the antivenom is rarely used because of its side effects, horses are still used to produce new batches of the medicine, which expires after 2 years.











![Hotstar Premium Cookies 2019 [*100% Working & Daily Updated*] Hotstar Premium Cookies 2019 [*100% Working & Daily Updated*]](https://tahav.com/wp-content/uploads/2019/11/Hotstar-Premium-Cookies-Free-100x70.jpg)




I love what you guys are up too. https://cavm-ombc.ca